Many of people believe they have a food
allergy because they react to a food in some way. However, most of the time
it’s not an actual allergy but sensitivity to the food they are experiencing. A
“true” allergy is where there is an IgE mediated immune reaction within the
body. These allergies affect about two to three percent of the population
only.
An IgE allergy reaction can result
in symptoms such as a rash or hives and can also be as drastic as anaphylaxis
which is where the mouth and tongue swell along with constriction of the
airways. People diagnosed with this type of allergy carry an EpiPen with them
in case of exposure as extreme reactions are life threatening. An IgE reaction
is usually noticed very soon after consuming the food.
The most common allergy foods are peanuts,
tree nuts, eggs, soy products, dairy, wheat, oranges, shellfish and fish.
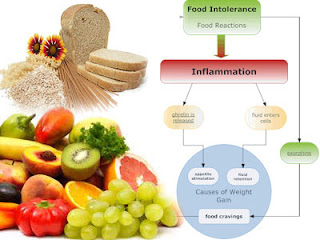
Food intolerance or sensitivity is where
the body has developed an IgG mediated immune reaction to a food. This is where
IgG antibodies are created in the body after it recognises the protein in that
food as an allergen or “enemy”.
Symptoms of food intolerances are wide and
varied and can affect any of the body systems from digestive problems, skin
problems, mood and behavior changes, respiratory reactions, muscle aches and
pains and much more. Different from IgE reactions, IgG reactions can take some
hours and sometimes up to a couple of days to surface which makes it even more
difficult to determine without good food detective work.
Testing for food reactions should start
with IgE blood testing to check for true allergies to rule these out. Then a
blood spot (finger prick collection) or serum (vein blood collection) test can
be carried out for IgG reaction to foods.
There is also another type of food
intolerance test that I use and this is ALCAT testing. This is where a blood
sample is collected (vein) and sent to the pathology laboratory overnight. The
blood is then exposed to various foods and the reaction of the white blood
cells are noted and recorded. The more active the white blood cells are the
more of a problem that food is to the body. Sometimes this test is preferable as it
reflects a reaction in the body to the whole food and not just the protein
component.
At the end of the day, aside from IgE test
results, the tests for food intolerances are there as a guide. For example you
need to be eating a good range of foods leading up to intolerance testing for
the test results to be as accurate as possible. If for example you haven’t
eaten a food for some time, that food is unlikely to present as an intolerance during
the test because the body would not be recognising it as a problem.
Although very time consuming and fraught
with difficulties in social situations, strict food elimination for a time
followed by single food re-introduction to “challenge” the body is the most
accurate way to determine food intolerances. This method takes quite
some time and persistence. Most people prefer to have results quickly and this
is where food intolerance testing can really help speed the process. Because of
this I use food intolerance testing in its various forms on a regular basis in
my practice. My patients find it very helpful in pinpointing problem foods to
reduce their symptoms from the outset. I find this approach along with detailed
food-diary recording excellent for spotting problem foods or drinks to speed my
patient’s way to better health.
If you're having problems with foods and would like to discover which are the most problematic come and see me for a consultation.